
نشریه علمی پژوهشی طب انتظامی Journal of Police Medicine

Volume 11, Issue 1 (2022)
J Police Med 2022, 11(1) |
Back to browse issues page
Ethics code: IR.SHAHED.REC.1400.173
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Vaseie M, Amini M, Tavasoli M M. Comparative Study of the Findings of the First Complete Blood Cell Count in Determining the Outcome of Patients with Covid-19: A Cross-Sectional Study. J Police Med 2022; 11 (1) : e32
URL: http://jpmed.ir/article-1-1107-en.html
URL: http://jpmed.ir/article-1-1107-en.html
1- Department of Emergency Medicine, Faculty of Medicine, Tehran University of Medical Sciences, Tehran, Iran
2- Department of Infectious Diseases & Tropical Medicine, Faculty of Medicine, Shahed University, Tehran, Iran , mamini@shahed.ac.ir
3- Department of Infectious Diseases & Tropical Medicine, Faculty of Medicine, Shahed University, Tehran, Iran
2- Department of Infectious Diseases & Tropical Medicine, Faculty of Medicine, Shahed University, Tehran, Iran , mamini@shahed.ac.ir
3- Department of Infectious Diseases & Tropical Medicine, Faculty of Medicine, Shahed University, Tehran, Iran
English Extended Abstract: (1060 Views)
INTRODUCTION ... [1-4]. The primary infection and pathogenesis of Covid-19 are still unknown, but in most patients, it causes lung involvement and mainly respiratory disease [5]. ... [6]. Currently, the gold standard for the diagnosis of Covid-19 patients is the detection of SARS-CoV-2 nucleic acid by real-time reverse transcription polymerase chain reaction (RT-PCR) from respiratory samples (oral and nasopharyngeal swabs) [7, 8]. Based on studies conducted in China and elsewhere, clinical hematology tests play an essential role by providing useful prognostic markers to the clinical team, so they can be helpful in the triage and management of affected patients [9]. Some laboratory abnormalities include decrease in the number of white blood cells and lymphocytes, neutrophilia, thrombocytopenia, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), and abnormal procalcitonin (PCT) in most patients. Also, the blood count of patients with covid-19 infection at the time of diagnosis shows changes related to the disease's stage and severity [6, 10]. AIM(S) This study aimed to compare the findings of the first CBC-Diff in discharged patients with a diagnosis of Covid-19 compared to those who died in Shahid Mostafa Khomeini Hospital. RESEARCH TYPE This is a cross-sectional study. RESEARCH SOCIETY, PLACE & TIME Using the census sampling method, the files of all patients hospitalized in the adult department of Mustafa Khomeini Hospital with a definite diagnosis of Covid-19 who were hospitalized between March 2019 and October 2021 were collected, and the survival of the patients was followed up to one month after discharge. USED DEVICES & MATERIALS In terms of net and composite results, the first CBC-Diff laboratory finding was evaluated, and the survival time was one month after discharge, personally followed by the researcher. The CBC-Diff test was performed by the Sysmex kx21 cell counter made in Japan after calibration according to the manufacturer's standard, and a laboratory science expert reported all the results of the CBC-Diff test. Definite diagnosis of covid-19 was done by RT-PCR test and SARS-CoV-2 IgG Detection kit in ELISA test of Pishtaz Co with the license of Ministry of Health ISO13485. METHOD By referring to the medical record archive section of the hospital, demographic information and the first CBC-Diff laboratory finding of all patients with a definite diagnosis of Covid-19 were extracted. Then, the information of the patients who met the conditions for entering the study was extracted, and the files that were incomplete in this respect were excluded from the study. Based on the form, information including items such as age, sex, body mass index, hospitalization date, discharge or death date, underlying diseases, and the results of the first laboratory findings (CBC-DiffWBC, HBG, MCV, RDW, MCH, Eosinophil, Neutrophil, Lymphocyte, Monocyte, Platelet NLR, PLR, SII) was prepared, and finally, the information included two general sections of demographic questions and laboratory results related to the research objectives. The normal level of measured parameters is as follows: WBC=4.8-10.8×1000/MICL, Hemoglobin=12-16 g/dl, RDW-CV=11.5-16%, Neutrophil=55-75%, Lymphocyte=20-40%, Monocytes=1-8%, EOSINOPHIL=1-5%) ETHICAL PERMISSION This study was conducted after obtaining the code of ethics as IR.SHAHED.REC.1400.173. STATISTICAL ANALYSIS All the obtained data were collected in Excel 2013 software. Data were analyzed using Medcalc 2013 statistical software. Combined data were calculated based on standard formulas (PLR=Platelet/Lymphocyte, NLR=Neutrophil/Lymphocyte, SII=Platelet×NLR). The normality of the distribution of the variables was checked based on the Shapiro-Wilk test. Due to the fact that the dependent variable was quantitative, the binomial logistic regression model was used considering the assumptions of the above test (the dependent variable is two-state, the quantitative data should have a linear relation with the independent variables based on the Box-Tidwell test). First demographic variables were measured from the confounding by Multivariate regression analysis. The chance or survival event was then calculated based on the absolute and composite results of the first CBC-Diff laboratory finding. The fit of the model was measured based on the Hosmer-Lemeshow test. Also, the number of changes in the independent variable (parameters of the first laboratory finding CBC-Diff) on the dependent variable (survival) was measured using the Cox & Snell R2 and Nagelkerke R² tests. The p-value was less than 0.05 as the significance criterion. FINDING by TEXT Finally, after removing the incomplete files, the data of 213 adult patients were analyzed. In the discharged group of this study, 77 women (55.6%), 61 men (44.4%) with an average age of 60.96±17.37 years, and in the dead group, 34 women (45.7%) and 41 men (54.3%) with an average age of 57.71±14.74 years were studied. Demographic indicators and the first CBC-Diff laboratory findings of the study population are summarized in Table 1. The dispersion distribution of demographic indicators and laboratory findings was statistically evaluated using the Shapiro-Wilk test. Other indices did not have a normal distribution except for the hemoglobin index. In the dead group, 16 patients had no body mass index. One patient did not have neutrophils, lymphocytes, Eosinophils, and monocytes indicators. In the discharged group, 20 patients had body mass index, six had RDW index, and one did not have neutrophils, lymphocytes, Eosinophils, and monocytes indicators. Of the 138 discharged patients, 32% had a history of diabetes, 28% had a history of heart disease, 12% had a history of other diseases (addiction, thyroid, respiratory, kidney), and 28% had no underlying diseases. Of the 75 dead patients, 56% were women, 31% had a history of diabetes, 36% had a history of heart disease, 12% had a history of other underlying diseases (addiction, thyroid, respiratory, kidney), and 21% had no underlying diseases (Table 1). For the correlation of demographic factors (gender, underlying disease, age, and body mass index) of hospitalized patients diagnosed with covid-19 using the logistic regression model, it can be said that none of the demographic factors affected the chance of survival. Cox-Snell's coefficients and Nagelkerk's test showed that demographic factors affected the chance of survival from 16.9 to 23.5%, which was not significant. Also, the Box-Tidwell test showed a linear relationship between the quantitative independent variable (age and body mass index) and did not need to be categorized. In general, it can be said that none of the demographic factors were confounding (Table 2). To relate the first hematology findings on the survival of patients with covid-19 infection (WBC, HGB, MCV, RDW, MCH, PLT, Eosinophils, Neutrophils, Lymphocyte, Monocytes) hospitalized patients diagnosed with covid-19. Using a logistic regression model simultaneously, it can be said that the increase of WBC with a cut-off point higher than 9×1000/micl was adequate. Its detection power was weak (ROC=0.66, p=0.001, X²=21.82). Hemoglobin decrease with a cut-off point of 11.1g/dl was effective and lacked diagnostic power (ROC=0.58, p=0.03, X²=4.33). The increase in RDW with a cut-off point higher than 14.6% was effective, and its diagnostic power was weak (ROC=0.66, p=0.002, X²=13.83). The increase of MCH with a cut point higher than 27.1 pg was ineffective and lacked diagnostic power (ROC=0.54, p=0.12, X²=2.35). MCV increase with a cut point higher than 83.3 fl was effective, and its diagnostic power was weak (ROC=0.60, p=0.02, X²=4.94). Platelet increase with a cut-off point of less than 259×1000/micl was ineffective and lacked diagnostic power (ROC=0.50, p=0.60, X²=0.26) (Figure 1). Eosinophil increase with a cut-off point of less than 1% was ineffective and had no diagnostic power (ROC=0.54, p=0.71, X²=0.13). The increase of neutrophils with a cut-off point of more than 79% was effective and had good diagnostic power (ROC=0.70, p=0.001, X²=19.66) (Figure 2). Lymphocyte reduction with a more than 14% cut-off point was effective and had good diagnostic power (ROC=0.70, p=0.001 X²=24.16). The reduction of monocytes with a cut-off point of less than 3% was ineffective and had no diagnostic power (ROC=0.55, p=0.13, X²=2.24) (Figure 3). Increasing the ratio of neutrophils to lymphocytes with a cut-off point of more than 5.6% was effective and had good diagnostic power (ROC=0.70, p=0.001, X²=28.78). The increase in the ratio of platelets to lymphocytes with a cut-off point of more than 10.16 was effective and had poor diagnostic power (ROC=0.67, p=0.001, X²=16.50). An increase in the immune-inflammatory system index with a cut-off point of more than 945 was effective and had poor diagnostic power (ROC=0.68, p=0.001, X²=17.72) (Figure 4). Based on the study's findings, the table of sensitivity and specificity of hematology markers was extracted (Table 3). MAIN COMPARISION to the SIMILAR STUDIES This study showed that the first hematology findings for prognosis and predicting the survival of patients with covid-19 infection are the increase of neutrophils and the increase of neutrophil to lymphocyte ratio. These markers had good diagnostic power. Lanini et al.'s 2020 study titled "Covid-19 disease, temporal analysis of complete blood count parameters during illness and association with patient demographics and management outcomes in survivors and deaths. A longitudinal descriptive cohort study" conducted in Italy on CBC laboratory results of 379 patients with Covid-19 for 21 consecutive days shows that 10.8% of patients died and 89.2% of patients were discharged. Gender (245 men, 93 women in the discharged group and 28 men, 13 women in the deceased group) does not affect the frequency of death, but age (over 60 years vs. 60 years or less) affects the frequency of death. Underlying diabetes and heart disease (34 people vs. 11 people, 102 people vs. 27 people) affects the frequency of death. The first laboratory results of CBC showed that high neutrophils and low lymphocytes affect the frequency of death. The decrease of monocytes has no effect, the decrease of hemoglobin has no effect, the increase of MCV has no effect, the increase of RDW has an effect, and the increase of platelets has an effect [15, 16]. Regarding gender, high neutrophil, low lymphocyte, and increased RDW were consistent with the present study. However, the results of the underlying disease and increased platelets were not consistent with the present study [17]. The difference can be in the type of race and the severity of the disease. The death rate of the present study was 35.2%. Liu et al.'s 2020 study titled "Development and Validation of a Risk Score Using Complete Blood Count to Predict Hospital Mortality in Covid-19 Patients” conducted in Italy and China on 9084 infected patients shows that based on the first findings of the CBC test, the five risk factors for death are platelets, white blood cells above 9.5, neutrophils and lymphocytes, and old age. This result was consistent with the current study regarding white blood cells, neutrophils, and lymphocytes (both from the cut-off point of death estimation and the type of relationship). However, it was not consistent in terms of platelets. In the case of platelet incompatibility, it can be said that the cut-off point is selected in the estimation of death. In the mentioned study, the cut-off point was less than 125, but in the present study, it was less than 259,000 micro/liter, and the frequency of death was 8.5% in the above study and 35% in the present study [18]. Mousavi et al.'s study was conducted in Tehran on 225 patients with covid-19, which shows that 24.4% of patients died, and based on the first findings of the CBC test, three risk factors have been identified for death, high lymphocytes, low neutrophils, and decreased hemoglobin [19]. In terms of demographic indicators, gender was not influential. However, age was influential, entirely consistent with the present study regarding lymphocytes and neutrophils, but not in hemoglobin reduction. In case of inconsistency, it can be said that it is a particular cut-off point in the estimation of death. In the above study, the cut-off point was less than 12g/dL, but in the present study, it was less than 11.1 g/dL. Bahl et al.'s study in 2020 was conducted on 1461 patients with covid-19 and showed that 22.4% of patients died due to covid-19. Age and body mass index affect the frequency of death. However, gender has no effect, and based on the first findings of the CBC test, the four risk factors of death are high platelets, white blood cells, lymphocytes, and low hemoglobin [20] in terms of gender, age, high white blood cell, high lymphocyte was consistent with the present study. However, it was not consistent in high platelet and low hemoglobin. The inconsistency can be attributed to the large sample size of the above study. In the present study, hemoglobin drop and platelet increase were more observed in deceased people, but it was not significant. LIMITATIONS The most important limitation of this study was the incompleteness of the information in the patients' files. Although the intended study was cross-sectional, due to space and time limitations, it was only possible to examine some of the causes of intervention. SUGGESTIONS Future studies with a larger statistical population and broader geographical survey will lead to the possibility of obtaining accurate results. CONCLUSIONS The three factors of increasing neutrophils, decreasing lymphocytes, and increasing the ratio of neutrophils to lymphocytes are good predictors for detecting death in Covid-19. CLINICAL & PRACTICAL TIPS in POLICE MEDICINE In this study, an attempt was made to gather valuable and brief information about covid-19 by examining hematological factors. Considering the spread of Covid-19 in high-density environments such as military barracks, this article emphasizes quick recognition of the mentioned cases. Considering the predictive cases of death in those suffering from covid-19, equipping the laboratories of military centers for the rapid preparation of laboratory results according to the cases explained above can play an essential role in the rapid recognition and treatment of high-risk individuals. ACKNOWLEDGMENTS The cooperation of Mustafa Khomeini Hospital staff in completing this project is appreciated. CONFLICT of INTEREST The authors state that the present study has no conflict of interest. FUNDING SOURCES This project was done with the financial support of Shahed University.
Table 1) Descriptive-quantitative frequency of demographic indicators and the first laboratory findings of CBC-Diff in hospitalized patients who died/discharged the diagnosis of Covid-19 from March 2018 to October 2020
| Indicator | deceased people | Discharged people |
Distribution | P-VALUE | ||||||
| number | mean | Standard deviation | CI:95% | number | mean | Standard deviation | CI:95% | |||
| age (years) | 75 | 75.17 | 14.74 | 14.74±29.48 | 138 | 60.96 | 17.38 | 96.60±34.54 | abnormal | 0.25 |
| BMI (Kg/m2) | 59 | 25.84 | 5.17 | 25.8±10.34 | 118 | 27.38 | 4.79 | 27.38±9.4 | abnormal | 0.068 |
| WBC (×1000 μl) | 75 | 10.06 | 5.41 | 10.06±10.82 | 138 | 7.28 | 2.91 | 7.28±5.82 | abnormal | 0.26 |
| HGB(g/dL) | 75 | 12.54 | 2.23 | 10.54±4.46 | 138 | 13.16 | 1.96 | 13.16±6.3 | normal | 0.002 |
| MCV(fl) | 75 | 85.28 | 6.19 | 85.2±12.38 | 138 | 83.01 | 7.76 | 83.01±15.26 | abnormal | 0.32 |
| RDW (%) | 75 | 15.52 | 2.45 | 4.90±31.4 | 132 | 14.36 | 1.64 | 14.36±3.28 | abnormal | 0.68 |
| MCH(pg) | 75 | 28.73 | 3.64 | 28.37±7.28 | 138 | 27.99 | 3.27 | 27.99±6.54 | abnormal | 0.32 |
| PLT (×1000 micl) | 75 | 201.24 | 95.26 | 201.24±192.2 | 138 | 195.40 | 68.46 | 195.40±169.8 | abnormal | 0.003 |
| Eosinophils (%) | 74 | 1.86 | 2.90 | 1.86±5.8 | 138 | 1.75 | 1.18 | 1.75±2.36 | abnormal | 0.35 |
| Neutrophils (%) | 74 | 81.08 | 10.11 | 81.08±20.22 | 137 | 74.57 | 10.41 | 74.57±20.82 | abnormal | 0.69 |
| Lymphocyte (%) | 74 | 14.59 | 8.06 | 14.59±16.12 | 137 | 20.91 | 9.42 | 20.91±18.84 | abnormal | 0.001 |
| Monocytes (%) | 74 | 2.45 | 1.34 | 2.45±2.68 | 137 | 2.76 | 1.43 | 2.76±2.86 | abnormal | 0.002 |
| NLR | 74 | 7.91 | 5.38 | 7.91±10.58 | 137 | 4.68 | 2.92 | 4.68±5.4 | abnormal | 0.003 |
| PLR | 74 | 18.07 | 13.10 | 18.07±26.20 | 137 | 11.93 | 8.12 | 11.93±16.24 | abnormal | 0.004 |
| Sll | 74 | 1533.27 | 1223.30 | 1533.27±144.606 | 137 | 946.33 | 739.15 | 946.33±8714.30 | abnormal | 0.027 |
Table 2) Relation of demographic factors on the survival of hospitalized patients diagnosed with covid-19
| survive | Estimation | percent | ||||
| discharge | death | |||||
| observation | discharge | 78 | 40 | 66.1 | ||
| death | 22 | 37 | 62.7 | |||
| correctness | 65 | |||||
| logistic regression | X2(6)=32.85,P=0.001 Cox & Snell R Square=0.169 Nagelkerke R Square=0.235 |
|||||
| Indicator | B | S.E. | Wald | df | p | Exp(B) |
| Gender (male to female) | 0.03 | 0.36 | 0.01 | 1 | 0.91 | 1.03 |
| underlying disease (not having) | 0.53 | 0.49 | 1.16 | 1 | 0.28 | 1.70 |
| age (years) | 0.42 | 0.48 | 0.77 | 1 | 0.37 | 1.53 |
| Age interaction (Box-Tidwell) | -0.07 | 0.09 | 0.58 | 1 | 0.44 | 0.93 |
| Body mass (Kg/m2) | -2.03 | 1.43 | 1.99 | 1 | 0.15 | 0.13 |
| Body mass interaction (Box-Tidwell) | 0.46 | 0.33 | 1.95 | 1 | 0.16 | 1.59 |
| width from the origin (constant factor) | 3.96 | 1.16 | 0.15 | 1 | 0.69 | 51.81 |


Figure 1) Determination of cut-off point and sensitivity and specificity of hematology markers
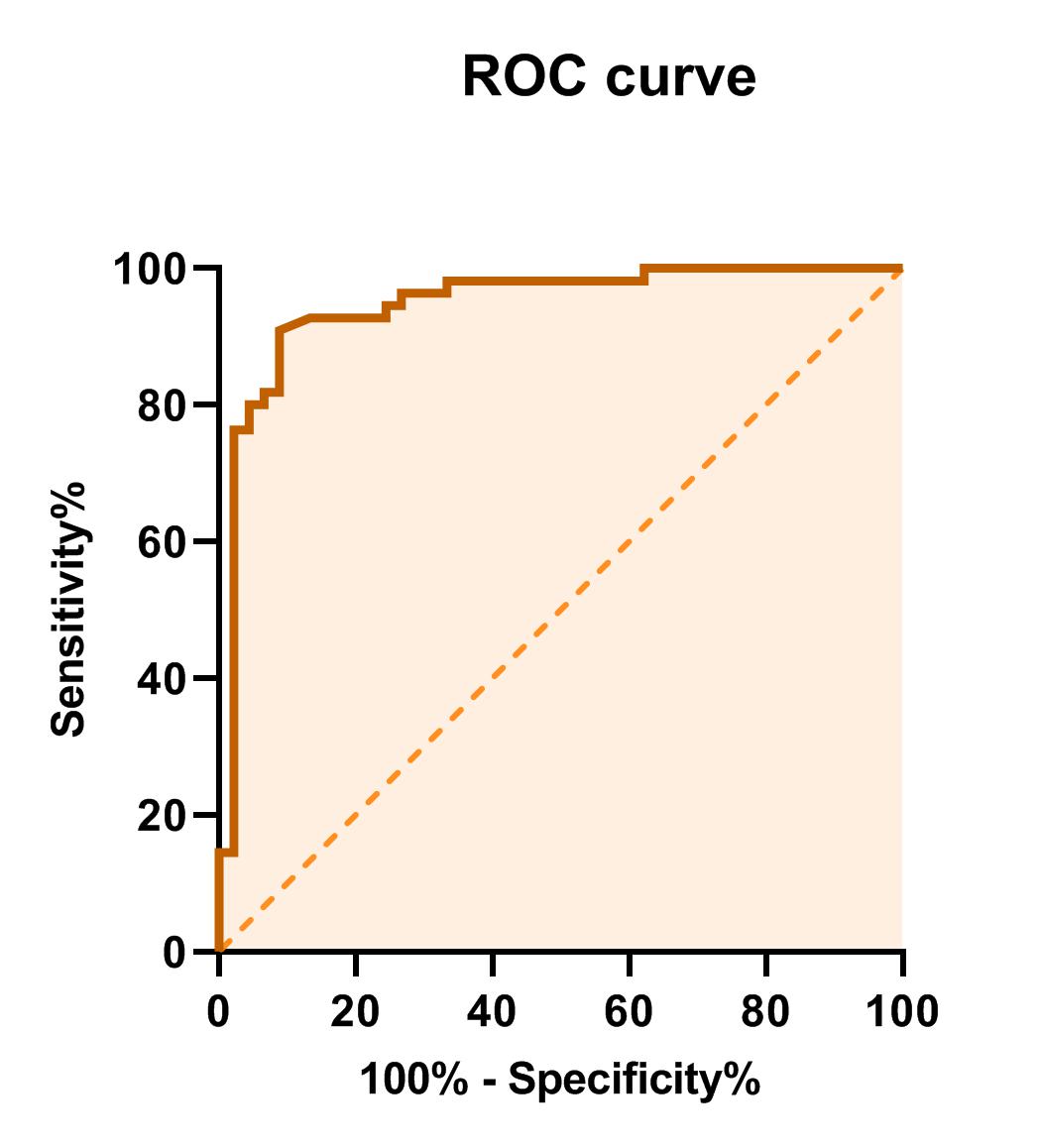
Figure 2) ROC curve for Neutrophil-Lymphocyte Ratio index

Figure 3) Determining the cut-off point and sensitivity and specificity of hematology markers



Figure 4) Determining the cutoff point and sensitivity and specificity of hematology markers
Table 3) Sensitivity and specificity of hematology markers
| Index | Sensitivity | specificity |
| WBC (×1000 micl) | 54.7 | 90 |
| HGB (g/dl) | 30.7 | 92 |
| MCV (fl) | 73.3 | 51.4 |
| RDW (%) | 87.7 | 71.7 |
| MCH (pg) | 80 | 29.7 |
| PLT (×1000 micl) | 70.7 | 12.3 |
| Neutrophils (%) | 74.4 | 27.7 |
| Lymphocyte (%) | 60.8 | 70 |
| Monocytes (%) | 40.5 | 67.9 |
| NLR | 62.2 | 73 |
| PLR | 75.7 | 54.7 |
| SII | 68.6 | 63.5 |
Article number: e32
Article Type: Original Research |
Subject:
Urban Epidemiology
Received: 2022/06/22 | Accepted: 2022/09/26 | Published: 2022/10/17
Received: 2022/06/22 | Accepted: 2022/09/26 | Published: 2022/10/17
References
1. Chan J.F.W, Kok K.H, Zhu Z, Chu H To, K.K.W Yuan, S Yuen, K.Y. Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. Emerg. Microbes Infect. 2020;9:221-36.
https://doi.org/10.1080/22221751.2020.1719902 [DOI:10.1080%2F22221751.2020.1719902] [PMID] [PMCID]
2. Mena G, Martinez P.P, Mahmud A.S, Marquet P.A, Buckee C.O, Santillana M. Socioeconomic status determines COVID-19 incidence and related mortality in Santiago, Chile. Science 2021;372(6545):eabg5298.
https://doi.org/10.1126/science.abg5298 [DOI:10.1126%2Fscience.abg5298] [PMID] [PMCID]
3. Keddie S, Ziff O, Chou M.K, Taylor R.L, Heslegrave A, Garr E, Lakdawala N, Church A, Ludwig D, Manson J et al. Laboratory biomarkers associated with COVID-19 severity and management. Clin. Immunol. 2020;221:108614. [DOI:10.1016/j.clim.2020.108614] [PMID] [PMCID]
4. Zeng Z.Y, Feng S.D, Chen G.P, Wu J.N. Predictive value of the neutrophil to lymphocyte ratio for disease deterioration and serious adverse outcomes in patients with COVID-19, a prospective cohort study. BMC Infect. Dis. 2021;21(1): 80. [DOI:10.1186/s12879-021-05796-3] [PMID] [PMCID]
5. Zhu Z, Cai T, Fan L, Lou K, Hua X, Huang Z. Clinical value of immune-inflammatory parameters to assess the severity of coronavirus disease 2019. Int J Infect Dis. 2020;95:332-9. [DOI:10.1016/j.ijid.2020.04.041] [PMID] [PMCID]
6. Liu Y, Du X, Chen J, Jin Y, Peng L, Wang H.H.X. Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalized patients with COVID-19. J Infect. 2020;81(1):e6-e12. [DOI:10.1016/j.jinf.2020.04.002] [PMID] [PMCID]
7. Huang Z, Fu Z, Huang W, Huang K. Prognostic value of neutrophil-to-lymphocyte ratio in sepsis: A meta-analysis. Am J Emerg. Med. 2020;38(3):641-7. [DOI:10.1016/j.ajem.2019.10.023] [PMID]
8. Kaushik R, Gupta M, Sharma M Jash D, Jain N, Sinha N. Diagnostic and Prognostic Role of Neutrophil-to-Lymphocyte Ratio in Early and Late Phase of Sepsis. Indian J Crit. Care Med. 2018;22(9):660-3.
https://doi.org/10.4103/ijccm.IJCCM_59_18 [DOI:10.4103/ijccm.ijccm_59_18] [PMID] [PMCID]
9. Farkas J, PulmCrit Neutrophil-Lymphocyte Ratio (NLR): Free Upgrade to Your WBC. Available online: https://emcrit.org/ pulmcrit/nlr/ (accessed on 1 October 2020).
10. Qin C, Zhou L, Hu Z, Zhang S, Yang S, Tao Y. Dysregulation of immune response in patients with COVID-19 in Wuhan. China. Clin Infect Dis. 2020;71:762-8. [DOI:10.1093/cid/ciaa248] [PMID] [PMCID]
11. Liu F, Zhang Q, Huang C, Shi C, Wang L, Shi N. CT quantification of pneumonia lesions in early days predicts progression to severe illness in a cohort of COVID-19 patients. Theranostics 2020;10(12):5613-5622.
https://doi.org/10.7150/thno.45985 [DOI:10.7150%2Fthno.45985] [PMID] [PMCID]
12. Yang A-P, Liu J.-P, Tao W.-Q, Li H-M. The diagnostic and predictive role of NLR, d-NLR and PLR in COVID-19 patients. Int Immunopharmacol. 2020;84:106504. [DOI:10.1016/j.intimp.2020.106504] [PMID] [PMCID]
13. Shang W, Dong J, Ren Y, Tian M, Li W, Hu J. The value of clinical parameters in predicting the severity of COVID-19. J. Med. Virol. 2020;92:2188-92. [DOI:10.1002/jmv.26031] [PMID] [PMCID]
14. Yan X, Li F, Wang X, Yan J, Zhu F, Tang S. Neutrophil to lymphocyte ratio as prognostic and predictive factor in patients with coronavirus disease 2019, A retrospective cross-sectional study. J Med Virol. 2020;92:2573-81. [DOI:10.1002/jmv.26061] [PMID] [PMCID]
15. Ulloque-Badaracco J.R, Ivan Salas-Tello W, Al-kassab-Córdova A, Alarcón-Braga E.A, Benites-Zapata V.A, Maguiña J.L, Hernandez A.V. Prognostic value of neutrophil-to-lymphocyte ratio in COVID-19 patients: A systematic review and meta-analysis. Int J Clin Pract. 2021;75:e14596. [DOI:10.1111/ijcp.14596] [PMID]
16. Soraya GV, Ulhaq ZS. Crucial laboratory parameters in COVID-19 diagnosis and prognosis: an updated meta-analysis. Medicina clinica. 2020;155(4):143-51. [DOI:10.1016/j.medcle.2020.05.004] [PMID] [PMCID]
17. Lanini S, Montaldo C, Nicastri E, Vairo F, Agrati C, Petrosillo N et al. COVID-19 disease-temporal analyses of complete blood count parameters over course of illness, and relationship to patient demographics and management outcomes in survivors and non-survivors: a longitudinal descriptive cohort study. PloS one. 2020;15(12):1-17. [DOI:10.1371/journal.pone.0244129] [PMID] [PMCID]
18. Liu H, Chen J, Yang Q, Lei F, Zhang C, Qin J-J et al. Development and validation of a risk score using complete blood count to predict in-hospital mortality in COVID-19 patients. Med J. 2021;2(4):435-47. [DOI:10.1016/j.medj.2020.12.013] [PMID] [PMCID]
19. Mousavi SA, Rad S, Rostami T, Rostami M, Mousavi SA, Mirhoseini SA. Hematologic predictors of mortality in hospitalized patients with COVID-19: a comparative study. Hematology. 2020;25(1):383-8. [DOI:10.1080/16078454.2020.1833435] [PMID]
20. Bahl A, Van Baalen MN, Ortiz L, Chen N-W, Todd C, Milad M et al. Early predictors of in-hospital mortality in patients with COVID-19 in a large American cohort. Intern Emerg Med. 2020;15(8):1485-99.
https://doi.org/10.1007/s11739-020-02509-7 [DOI:10.1007%2Fs11739-020-02509-7] [PMID] [PMCID]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |

